Author: Nikolay Kefilev, MD
Due to the ubiquitous presence of the sodium-potassium ATPase in the human body, any impairment of its function leads to a pathological distribution of the sodium and potassium located on the sides of the cellular and mitochondrial membranes for the cells of all organs and systems. Under such conditions, there is a serious impairment of the body's homeostasis, including a significant shift in water and electrolyte balance. When the function of the sodium-potassium pump is insufficient, there is a higher intracellular accumulation of sodium ions. The presence of an abnormal quantity of these ions leads to intracellular hyperhydration, and the development of edema within the cell. As such, its function is emphatically impeded.
Other than a base mechanism to support the water-electrolyte balance between the cells and the surrounding interstitium, the sodium-potassium pump is integrated into multiple executive and regulatory mechanisms that support the body's functional fitness.
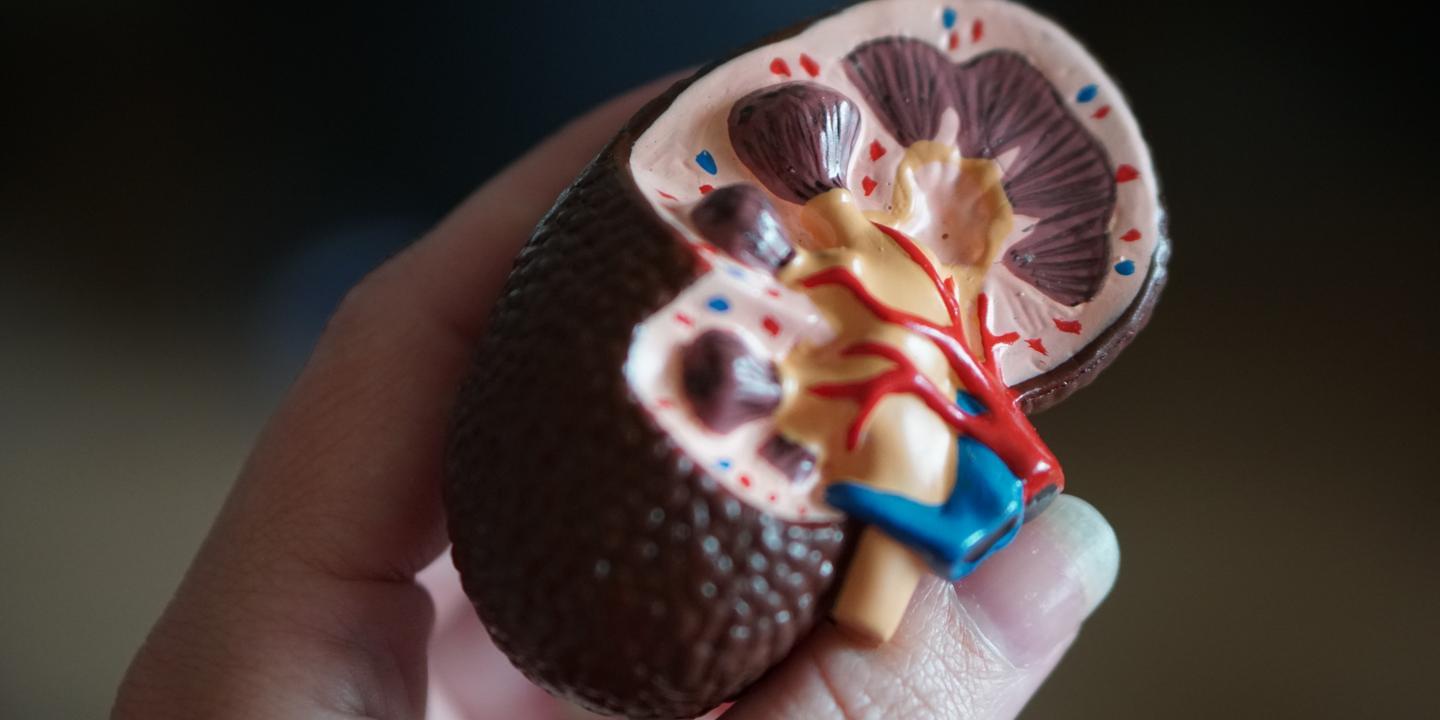
A stark demonstration of this is the pathological change which occurs on a renal level when this condition is present.
The role of the sodium-potassium ATPase in sodium's reabsorption on the renal tubular system level can be classified as key. The physiological mechanism which enacts the transportation of the sodium ion through the tubular epithelial cells includes the availability of an apically located active transport system where the cells intracellularly exchange hydrogen cations for the sodium ions located in the tubular lumen. The proper function of the sodium-potassium ATPase located in the part of tubular epithelial cells neighboring the vascular capillary peritubular network (basal part) is essential for the transfer of these sodium ions from the cell's interior into the renal capillary system. Through this sodium-potassium pump, the tubular epithelial cells transfer intracellular sodium to the underlying capillary system, exchanging it for potassium ions. When reviewing this physiological mechanism, it is important to note that the number of active apical Na-H+ exchangers is variable. The number of these exchangers depends directly to the blood and tissue levels of Angiotensin II. Some authors (1, p. 119) note that parallel with the number of apical transport units, Angiotensin II also regulates the activity of basally-located Na-K-ATPase.
In the pathogenesis of the condition currently under review, considering this physiological mechanism which prevents the renal loss of sodium ions for the body, there is an impeded reabsorption of approximately 65% of the sodium filtered through the renal glomerulus. This reabsorption is performed alongside the tubular system, starting from the proximal nephron tubule and reaching to the juxtaglomerular apparatus (JGA)'s macula densa. The impeded sodium reabsorption leads to elevated natriuria in the aforementioned sections of the nephron and ultimately leads to this a high concentration of sodium in the part of the urine which passes past the JGA's macula densa. Here I must remind that within the JGA's macula densa, there is a receptor system which links directly to the granular, renin-secreting cell located on the wall of the arteriole adducing to the renal glomerulus, neighboring the JGA. The receptor system in question, when registering a high sodium concentration in the urine filtrate (detects a combination of sodium concentration and urine discharge), induces suppression of the granular cell's renin secretion. This suppression leads to the development of basal reninemia or even hyporeninemia. As a result of this hyporeninemia, there is a chronic hypoangiotensin II-emia condition within the body. In turn, developing a hypoangiotensin II-emia condition reduces the amount of Na-H+ exchangers in the renal tubular epithelial cells and a reduces the sodium-potassium ATPase activity in those cells. This process results in a vicious cycle down the chain: Low NA-K-ATPase activity – high natriuria levels in the nephron's proximal end – suppression of renin secretion by the JGA and developing hyporeninemia – maintaining hypoangiotensin II-emia – low Na-H+ exchanger count in renal tubular epithelial cells – low sodium-potassium ATPase activity.
Aside from maintaining this vicious cycle which could lead to severe hyponatremia in the body, we should note the negative effect lowered blood and tissue levels of angiotensin II have over vascular spasm levels, their effect on renal microcirculation, over the entire body's interstitium, and the altered regulation of its dependent E-group prostaglandins. Before I proceed with describing the mineralocorticoid hormone (aldosterone)'s behavior, I should note that the altered state mentioned above matches the patient's clinical condition when they are not undergoing an episode, and there are no manifesting neurological symptoms of listlessness.
Here is another question of high importance. How does the mineralocorticoid hormone aldosterone behave in a chronic suppression state of the renin-angiotensin II system?
The answer to this question is related to the matter of physiological mechanism(s) that regulate the secretion of aldosterone. The largest portion of members of the medical, and possibly scientific community accept that the base regulation of aldosterone secretion is dependent on blood levels of renin and angiotensin II. In scientific medical literature, the following term has been introduced:
Renin-angiotensin-aldosterone system (RAAS), indicative of an accepted and backed by facts statement that elevation in reninemia, and therefore angiotensin-II-emia, consecutively leads to an increase of aldosteronemia. Does this mean that a pathological reduction of reninemia and angiotensin-II-emia would cause a pathological decline in aldosteronemia?
Patient tests are a clear demonstration of this. Tests indicate hyporeninemia and levels of aldosteronemia that are higher than those expected for such reninemia levels. The clinical laboratory where the tests were made set a reference threshold for the aldosterone/renin value ratio. This threshold is set at 20. Any elevation to the aldosterone/renin ratio beyond 20 is classified as an autonomous aldosterone secretion process. In such cases, we accept that there is elevated secretion of aldosterone which has been developed via other mechanisms, regardless of reninemia (respectively angiotensin-II-emia) levels. In such a patient you should therefore exclude primary hyperaldosteronism (Conn's syndrome). In the case under review, the presence of normal aldosterone blood levels accompanied by basal natremia values and values matching hyponatremia rule out the presence of an autonomous process in the patient's adrenal gland. The patient's tests from the latency period are proof that base aldosterone regulation is not related to reninemia and angiotensin-II-emia.
I should note here that "reduction of sodium in the serum is the main stimulus for aldosterone secretion" (2, p. 548).
In this specific case: chronically elevated hypernatriuria values in the nephron's proximal end (next to the distal convoluted tubule) poses a risk for the body of developing severe hyponatremia. The body's response in the event of a pathological decrease of natremia is to elevate the aldosteronemia via its base physiological regulation mechanism which doesn't include the renin-angiotensin II system. By elevating aldosteronemia as a result of a pathological natremia decrease, hyponatremia manages to approximate the base reference value. Clinical laboratory test analysis for this patient indicates that aldosteronemia levels compensate for the renin and angiotensin insufficiency when it comes to the developed hypernatriuria condition in the nephron's proximal end.
The significance of this phenomenon is two-fold.
First: By using the aldosterone secretion's base regulation mechanism, the body manages to protect itself from severe hyponatremia should there be a pathological substance decrease on the renin-angiotensin II chain.
Second: Clinical laboratory testing of natremia, reninemia, and aldosteronemia can be used as a credible noninvasive test to discover medical and pathophysiological conditions where elevated glomerulus filtration and decreased sodium reabsorption are present in the renal tubular system. The combination of base natremia and hyponatremia with base reninemia levels or the presence of hyporeninemia and elevated aldosteronemia/reninemia ratio values prove the presence of renin-angiotensin II system suppression.
From a medical and clinical point of view, I should note that the chronic base natremia and hyponatremia condition, when combined with base angiotensin II (and hypoangiotensin-II-emia) levels, leads to a chronic lack of thirst. The lack of thirst is a symptom which should be actively sought when taking the medical history of the parents of patients with alternating hemiplegia of childhood.